
Arthrosis is a joint degenerative pathology accompanied by dystrophy of cartilage. As the disease progresses, the articular sac, ligament, synovial membrane, and nearby bone structures become involved in the destructive process.
Prevalence of osteoarthritis
Most people with osteoarthritis are older people. After the age of 65, the disease is not only the most diagnosed joint pathology, but also the leading cause of disability with subsequent disability. In addition, women are more likely to be ill in old age, but the majority of young people are men.
The incidence of osteoarthritis varies greatly from country to country. It is not yet possible to determine the reasons for the widespread dissemination of statistics.
Causes and risk factors
Osteoarthritis is a disease that can be primary or secondary. If there are no objective reasons for the development of pathology, they talk about the main type. If it is possible to determine the causes of osteoarthritis, they talk about the second type.
Secondary osteoarthritis can be caused by the following negative factors:
- trauma to the joints of various natures (frequent falls, twists, bruises);
- chronic congenital tissue dysplasia;
- pathological changes in metabolic processes;
- various autoimmune pathologies;
- articular nonspecific inflammatory processes;
- some pathologies of the organs of the endocrine system;
- chronic degenerative-dystrophic processes;
- various diseases accompanied by a weak garden apparatus accompanied by excessive joint mobility;
- presence of hemophilia;
- specific inflammatory processes.
In addition to the immediate causes that lead to the development of osteoarthritis, there are also predisposing factors that do not cause the disease on its own, but may increase the risk of developing it.

These include:
- is over 55 years old;
- overweight due to increased load on the joints;
- Improper sports training, excessive load on any joint or group due to special work that requires a long stay in one position;
- history of joint surgery;
- heredity;
- hormonal changes in the female body in postmenopause;
- constant hypothermia;
- incurable pathologies of the spine;
- Insufficient intake of beneficial micro and macronutrients in food.
Development Mechanism
The mechanism of development of osteoarthritis is well known. The cartilage, which provides the normal contact of the two bones, helps to ensure normal movement in the joints, which is naturally smooth, without irregularities and roughness. With a disease, the structure of the cartilage changes, it becomes rougher, and there are defects on it that reduce the effect of natural sliding.
Due to the acquired inequality, cartilage is gradually damaged, begins to calcify in places, and in places becomes bone. In this case, it is possible to separate small particles that end up in the joint fluid and can damage the surrounding tissues.
As the pathology progresses, the joint may develop into a state of chronic subluxation, which will significantly impair motor function.
Degrees
Doctors divide osteoarthritis into three main degrees:
- I degree.It is characterized by the lack of a clear clinical picture. The patient may rarely complain of pain in the affected joint, but generally does not consult a doctor. At the same time, there are changes in the musculoskeletal system and articular fluid, but there are no visible deformations.
- II degree.The symptoms of osteoarthritis are more pronounced. The pain is characterized as tolerable, but occurs regularly. The patient consults a doctor because of a decrease in quality of life. A characteristic crisis is heard in the affected joint. Changes are observed in nearby muscle structures, as nerve conduction is impaired.
- III degree.It is characterized by the required symptoms. The joint cartilage is very thin, and cysts, calcifications, or foci of ossification can be found. The connective tissue of the garden is shortened, which leads to an increase in mobility in the affected area, which is accompanied by a restriction due to an open inflammatory process. The metabolism of the surrounding tissues suffers, which can lead to muscular dystrophy.
In any case, the patient needs to confirm the diagnosis from the attending physician. This is due to the specificity of the course of the disease, which is characterized by alternating and exacerbation stages.
Pain with illness

Pain in osteoarthritis is the most common complaint of patients. Their characteristic feature is the time of day, weather conditions, the relationship to physical activity.
In most patients, the pain is exacerbated by walking, running, or some other type of physical activity aimed at the affected joint. As the load stops, the pain gradually subsides. Their development is explained by the fact that the cartilage can no longer perform the functions of a shock absorber.
Anxiety at night is most often caused by blood stasis in the arteries. Another reason is the increase in intraosseous pressure during this period.
One of the main diagnostic criteria is the presence of so-called pain, which worries the patient as soon as he begins to move. If physical activity continues, the initial pain decreases. Their formation is explained by the presence of joint deposits (detritus) that irritate the nerve endings. As these deposits move away from the nerves, the pain disappears.
symptoms
In addition to pain, doctors also identify other symptoms of osteoarthritis, which can lead to suspicion of pathology.
These include:
- Painful and crunchy sound.Lomota mainly occurs when a person has hypothermia. The distress will be hard to hear at first, but it will be heard by those around you as the disease progresses without therapy.
- Decreased mobility. Mobility does not decrease in the early stages of pathology. However, the longer the disease is left untreated, the more severe the limitation of movement in the joint. This is explained by the narrowing of the joint space and the spasm of the nearest muscle structures.
- Joint deformation.It is characteristic of the final stage of osteoarthritis, but also an important indicator of the course of the disease. During this period, the disease is already very difficult to treat.
Which doctor treats osteoarthritis?
Who treats osteoarthritis? In most cases, several specialists are involved in therapy. First of all, an arthrologist, a joint specialist is involved. In addition, the patient needs to visit an orthopedist. If the disease is the result of an inflammatory process, it is advisable to consult a rheumatologist.
If necessary, other specialists may be involved during the treatment period. You often need to consult the services of traumatologists, physiotherapists, masseurs, surgeons.
Diagnostics
Treatment of osteoarthritis of the joints begins only after the diagnosis is confirmed and the pathological degree is determined. First of all, the doctor interviews and examines the patient in detail. The presence of characteristic complaints and deformities indicates a disease.
Radiography of the affected joint is a mandatory method to confirm the diagnosis. If the disease affects the knee, the knee is photographed, and if a pathological lesion is found, the radiological signs of the disease are specifically sought there.
Diagnosis using radiography does not always give sufficient results to diagnose the patient. In this case, it can be sent to MRI (this will allow to assess the condition of soft tissues and their involvement in the pathological process) or CT (this will allow to draw conclusions about the condition of bone and cartilage structures, the involvement of nearby anatomical structures in the pathological process).
Treatment
How to treat osteoarthritis of the joints? The choice of appropriate therapeutic technique depends on the severity of symptoms and the stage of the disease.
The doctor selects the therapy regimen after assessing the general condition of the patient and the course of the disease. Both conservative and surgical treatments can be used.
Medication
How can a disease be treated rather than using drugs rather than surgery?
Conservative therapy is suitable only for patients in the early stages of pathological development and covers the use of three main groups of drugs:
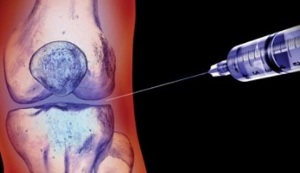
- glucocorticosteroids- hormonal drugs that effectively eliminate the inflammatory process during inflammation are injected into the joint cavity;
- Non-steroidal anti-inflammatory drugs,are usually injected into the muscles near the joint or directly into a vein. However, doctors may also recommend pills, although this choice to take NSAIDs is undesirable because of their adverse effects on the gastrointestinal tract;
- chondroprotectors- drugs of this group can reduce the destruction of cartilage tissue and enhance regeneration, especially effective in the early stages of the disease.
Surgery
If the disease is long enough, how is osteoarthritis treated? In this case, conservative therapy will be ineffective, and doctors can only offer surgery to the patient.
Today, most cases of endoprosthetic surgery are performed. During the operation, the real joint is replaced with a prosthesis that has all the functions of a healthy joint.
In some cases, palliative therapy options are offered, the main task of which is to reduce the load on the joint surfaces.
Sports
In the early stages of the disease is treated not only with drugs, but also with physiotherapy exercises. Exercise is an important part of therapy that helps maintain joint function and reduces the likelihood of developing the disease.
Depending on the severity of the pathology and the individual characteristics of the patient, the set of exercises is selected individually. The physician should consider the localization of the osteoarthritis, which allows the most effective effect on the affected tissues.
It is not recommended to work on your own without medical supervision, especially in the early stages. Exercises should be chosen to be as smooth as possible without sudden movements.
Sports therapy classes are effective only if the patient spends some time on the recommended complex each day.
Traditional methods

Many people who suffer from osteoarthritis refuse medication or surgery until the last moment. In this case, alternative drugs are used as a substitute for drugs.
The most commonly used herbs in therapy are:
- Kalanchoe;
- ginger;
- hell;
- bay leaf;
- garlic;
- cinnamon;
- ponytail, etc.
It is used in the form of tinctures, decoctions, spills on the affected area. It is important to remember that it is not possible to completely cure the disease using only home-made recipes. It is best if traditional treatments are combined with traditional medicine.
Prevention
What can be done to reduce the likelihood of developing osteoarthritis in old age? Simple preventive measures are available to everyone.
Recommended:
- moderate daily physical activity: walking, cycling, free simple exercises, etc.
- Follow the basic principles of healthy eating: eat often, but eat slowly, fast food, overeating, avoid heavy and fatty foods, eat a lot of spices;
- weight control: weight gain causes increased stress on the joints, which can lead to osteoarthritis;
- timely treatment of chronic diseases that cause metabolic disorders;
- Use of vitamin and mineral complexes when the amount of food provided is insufficient.
The difference between arthritis and osteoarthritis
Many people confuse arthritis and osteoarthritis due to the similarity of sound. But these are completely different diseases.
Arthritis is not a dystrophy or degeneration of the joint tissues, but any inflammatory reaction that can develop in the joint space, regardless of the cause. Inflammation affects not only the joint, but also the muscles, bones and ligaments closest to it. The pain in arthritis is not related to physical activity, it can bother the patient at rest, and there is no crisis in the joints.

In most cases, it is not possible to distinguish arthritis from osteoarthritis independently, because the main symptom is pain, and patients rarely imagine the specifics of each pathology.
In order not to make a mistake with the subsequent treatment and prevention of the disease, it is better to entrust an accurate diagnosis to the attending physician.
Arthrosis is a serious pathology that can lead to disability if the patient does not consult a doctor in time. At the first signs of the disease, it is advisable to contact a specialist to confirm the diagnosis and choose the most optimal treatment.
If it is possible to catch in the early stages of the disease, then it will be possible to do so without surgery, limited to conservative treatment.



































